‘First Gen’ Compassion To-Say List
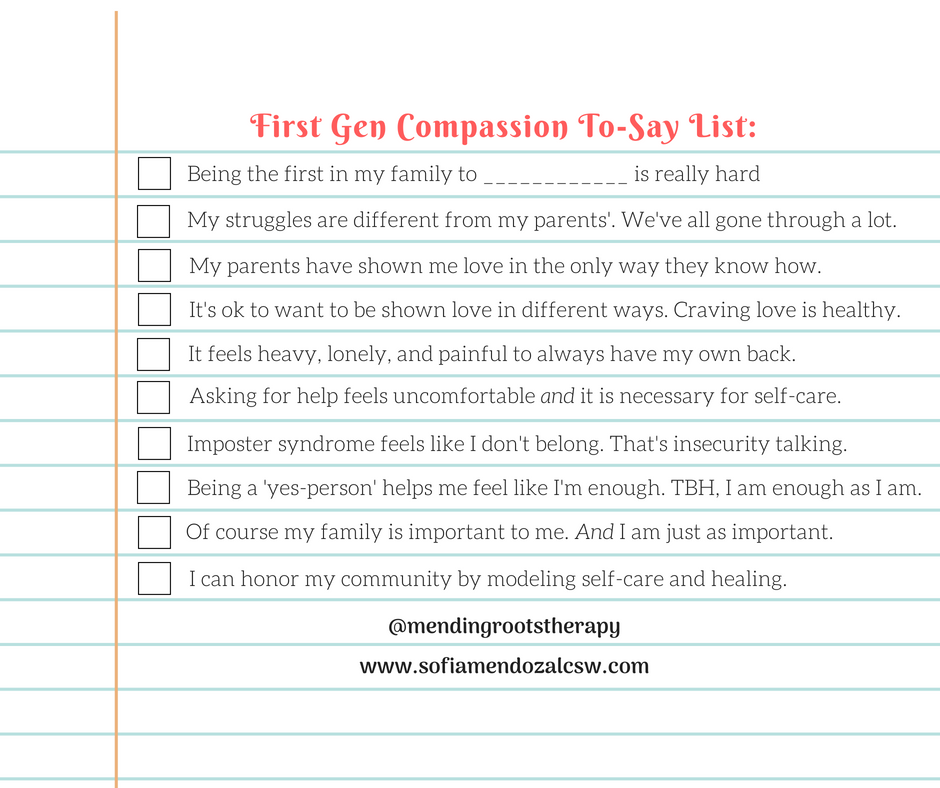
The term “First Gen” has become both a compassionate term of endearment and a resounding validation of experience. First Gen refers to First Generation – being the first in the family become a naturally born citizen in the United States. In my office, it also means First generation to take A.P. classes in high school, […]
Latinx Therapy Campaign: “Mental Health, it’s like the air that we breathe”
Today, I want to introduce you to the first ever National Latinx Campaign to reduce mental health stigma in the community. I am so thankful to Adriana Alejandre, LMFT for starting Latinx Therapy Podcast and the Latinx Therapy website/directory. The campaign’s mission is to 1) break the stigma of mental illness, 2) encourage our community […]
What do I say to my suicidal loved one?
I had the great honor to participate in an Instagram discussion on Mental Health and suicide within the POC (person of color), in particular the Latinx community. Check out the instagram account @thestrangeisbeautiful for the full conversation. There were 3 topics and I picked #1 to respond to as a mental health professional. Topic # […]
Your loved one is depressed. How to tell them about therapy

You’re sitting with your BFF (best friend forever) as she’s depressed, in tears and describing her extremely painful situation(s). You feel so much for her and also feel frozen. You don’t know what to do or say to make her feel better. All you know is you want her pain to end and don’t know […]
15 Statements to Convince Yourself to Self-Care: A love letter to all parents
“What to say” Series: Last week I wrote a blog post on 20 easy 5-minute self-care ideas for parents. Today, I continue the conversation in the guest post, “15 Statements to Convince Yourself to Self-Care: A love letter to all Parents” on The Productive Parent website. I provide 15 statements and quotes that parents […]
“I’m not bad…”
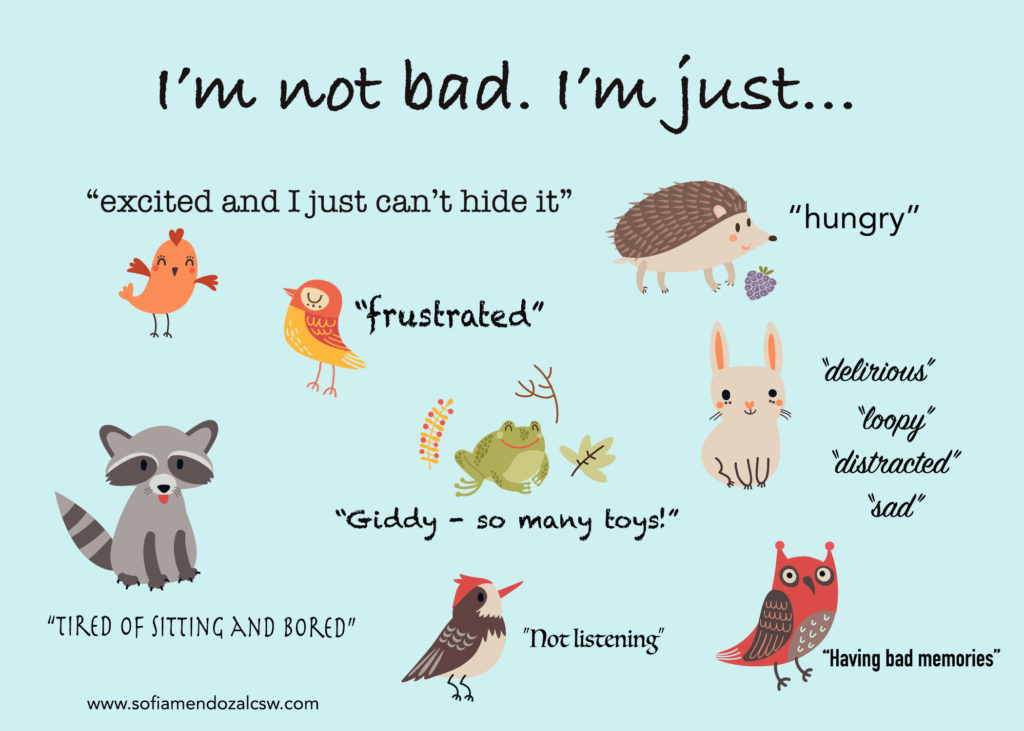
Ever want to shout out at a child, “Stop it, you’re being BAD?” You are definitely not alone. Parenting, caregiving, teaching children requires lots of patience and skill especially when they are not complying. Growing up, I knew a lot of kids who heard this from teachers, siblings, and well-meaning neighbors. These kids didn’t listen, […]
What to Say: It’s OK to not be OK
‘WHAT TO SAY’ Series: Recently mental health awareness efforts on social and public media have been growing exponentially. It makes me super happy that folks are talking about it from a public health perspective and making it’s way to people’s instagram, Facebook and Pinterest accounts and even music playlists as different artists are writing and […]

